A week after my prophylactic bilateral salpingo-oophorectomy (BSO) and total hysterectomy, I’m happy to report that I also said NOPE to ovarian cancer .. and uterine cancer and cervical cancer.
When my then-28-year-old sister was diagnosed with aggressive breast cancer in 2001, and died less than a year later, my world was rocked, but I had no idea just how rocky it would get. Since then there have been countless doctor’s visits, screenings, blood tests, anxious days and nights, and a few (!) surgeries. We’ve lost not only my sister, but my mom too, who was diagnosed with late-stage ovarian cancer and died in a year. 20 years later, I feel like I can finally breathe easier, like I’ve exhausted all the options available to me to greatly reduce my own risk of developing hereditary breast and ovarian cancer (HBOC).
I already made a decision to take some kind of action at 40. There were many options to be weighed and paths I could take. There’s an overwhelming amount of resources related to ovarian cancer testing, screening, treatment, and risk-reducing surgeries. Some are informative, others are eye-opening, and there are those that are terrifying. There were multiple questions to be answered if I was to move forward the surgical route:
 Do we take out both ovaries? Or just one and both fallopian tubes?
Do we take out both ovaries? Or just one and both fallopian tubes?- If two ovaries, will I use hormone replacement therapy (HRT) after?
- Should I also give the boot to my uterus?
- And if yes, what about the cervix?
In consulting with my husband, doctors and surgeons, including the gynecologic oncologist I have been seeing for years, we came to a decision and scheduled the surgery. On July 15, 2021 I underwent a procedure that removed both my ovaries and fallopian tubes as well as my whole uterus, including the cervix (so all of the above!). It was a robotic-assisted surgery, using the da Vinci system.

Artist: jcorres (redbubble.com)
It was a quick outpatient procedure, so I went home same day with four tiny incisions and an HRT patch. Since my surgery did include removal of ovaries, HRT will keep surgical menopause at bay. It delivers .1 mg/day of bio-identical estrogen. I’m only one week post-op, but so far so good – zero hot flashes to report! My body is still in shock, I think, and it may not all be peachy down the road, but I’ll deal as it comes. The recovery is not exactly a breeze (OMG, the gas pains!), but doesn’t even compare to that of the mastectomy, which was rough and long. I’m already off narcotics and back to doing some mobility workouts (easy peasy to start).
What’s next?
Over the coming days/months/years I will continue to visit my gynecologic oncologist for regular exams. We will work together to plan for the future and adjust as needed. And of course: eat healthy, exercise and meditate regularly, live clean, wear sunblock, and lay off the booze! At this point, I have some peace-of-mind in taking another step towards reducing my risk of the gynecological cancers that have affected my family. I’m doing what I can to say NOPE to breast and ovarian cancer!


 Although the tone of this post may not be entirely positive, I am in a good place. I feel great and still have no regrets about having the PBM. Somebody told me that it wouldn’t be easy and they were right. Totally worth it, though. However, I won’t say I’m done, because I’ve already declared that a couple of times and was wrong. We shall see where this goes. So far everything looks good.
Although the tone of this post may not be entirely positive, I am in a good place. I feel great and still have no regrets about having the PBM. Somebody told me that it wouldn’t be easy and they were right. Totally worth it, though. However, I won’t say I’m done, because I’ve already declared that a couple of times and was wrong. We shall see where this goes. So far everything looks good.







 I never really worried or thought much about cancer … until my sister was diagnosed with breast cancer at the age of 28. At the time, I was 21 years old, naive, in college, worried about what plans I had for the weekend, and didn’t really grasp what that meant. More than ten years later, my sister is gone, my mom is gone (ovarian cancer), my aunt is in treatment for colorectal cancer, my other sister just had her own scare, and although I am BRCA mutation uninformed negative, I underwent a prophylactic bilateral mastectomy and started the breast reconstruction process on January 22, 2013. I said NOPE to breast cancer.
I never really worried or thought much about cancer … until my sister was diagnosed with breast cancer at the age of 28. At the time, I was 21 years old, naive, in college, worried about what plans I had for the weekend, and didn’t really grasp what that meant. More than ten years later, my sister is gone, my mom is gone (ovarian cancer), my aunt is in treatment for colorectal cancer, my other sister just had her own scare, and although I am BRCA mutation uninformed negative, I underwent a prophylactic bilateral mastectomy and started the breast reconstruction process on January 22, 2013. I said NOPE to breast cancer.
 Greetings from NO FUN City
Greetings from NO FUN City



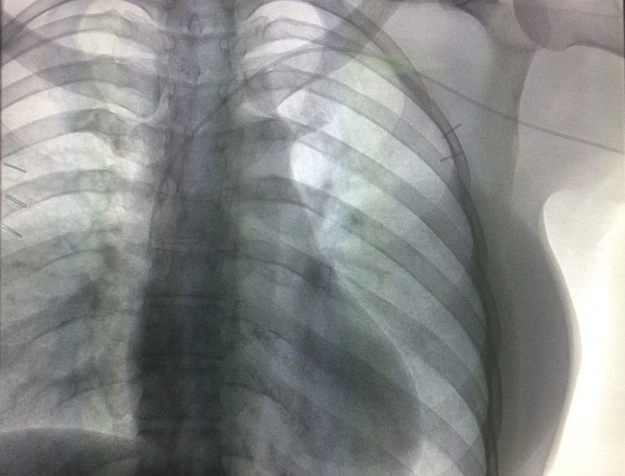
 I’m paranoid at this point, so I check things over a couple of times per day. Two weeks after my exchange surgery, I noticed a
I’m paranoid at this point, so I check things over a couple of times per day. Two weeks after my exchange surgery, I noticed a