Fitness, nutrition, and your health
Speaking of exercise … post-mastectomy exercises are crucial to a full, healthy, and speedy recovery. I keep mentioning Casey Eischen’s program, because it really is a great one and has been working well for me. Every day I do exercises and every day I get further than the day before.
 Click here if you’re interested in learning more or contacting Casey Eischen. This amazing lady 1. is a fitness expert and nutrition coach that is certified in training women who are recovering from breast cancer and related treatment or surgery, 2. she underwent a prophylactic bilateral mastectomy herself in November ’12, and 3. she took some time to provide invaluable feedback for this post. Also, be sure to visit (and like) Foobie Fitness, a FaceBook community page run by Casey Eischen.
Click here if you’re interested in learning more or contacting Casey Eischen. This amazing lady 1. is a fitness expert and nutrition coach that is certified in training women who are recovering from breast cancer and related treatment or surgery, 2. she underwent a prophylactic bilateral mastectomy herself in November ’12, and 3. she took some time to provide invaluable feedback for this post. Also, be sure to visit (and like) Foobie Fitness, a FaceBook community page run by Casey Eischen.
 Post-op workouts are one thing. Preparing your body before the procedure is another, and just as important. It is the #1 item on my preparing for surgery checklist: get in the best physical shape you can manage before the surgery. The healthier the body, the more tolerant it is to trauma, and the faster it recovers. I workout on a regular basis, however, I’m no fitness guru, so I would advise discussing exercise with your doctor and/or a certified trainer.
Post-op workouts are one thing. Preparing your body before the procedure is another, and just as important. It is the #1 item on my preparing for surgery checklist: get in the best physical shape you can manage before the surgery. The healthier the body, the more tolerant it is to trauma, and the faster it recovers. I workout on a regular basis, however, I’m no fitness guru, so I would advise discussing exercise with your doctor and/or a certified trainer.
In addition to physical fitness, nutrition is extremely important to aid healing and keep a hand on inflammation. According to Casey, Inflammation is attributed to the improper functioning of the immune system. Check out this meal plan she designed for Simple/Clean Nutrition.
Something that should go without saying – smoking is a big NO-NO.
Details

The breast reconstruction procedure utilizing expanders, and ultimately implants, wreaks havoc on the pectoralis major muscle. The nerves feeding the muscle are snipped when the pocket is created (note: this was the case with my PBM, but may not be the standard procedure for all plastic surgeons, so please talk to your doctor). This causes the muscle to atrophy and lose some of its functionality. The more developed the pec major, the more difficult (read: painful) the expansion process and following recovery will be. A few months before my prophylactic mastectomy, once I knew it was in my future, I began altering my routine. I stayed away from push ups and flys and instead focused on core and legs. After the procedure, because pec major is traumatized, core and legs must pick up the slack.
I’ve fallen and I can’t get up
Maya
My abs got me out of trouble on day three after the mastectomy. I was sitting on the floor petting a cat and decided it would be a good idea to lay down flat on the floor. That was fine and dandy until it was time to get up. No matter which way I tried to get up, I felt pain. Couldn’t roll over to my side, because I still had surgical drains coming out of me and I couldn’t use my arm to prop myself up if I ever got there. Bending at the waist was not working – my serratus was screaming. I finally wedged my feet under the couch and then used the leverage and my lower abs to bend at the waist.
It was scary as I was laying there helpless, but as soon as I managed to get up, I said to my self outloud: YOU F$@#ING IDIOT! It’s funny now, but wasn’t then. Moral of the story: don’t lie flat on your back three days after surgery, stupid.
 I have a desk job, so it isn’t very physically demanding, but I did feel completely pooped after my second day back. Sitting in one spot for most of eight hours is much different than lounging on the couch and it caught up with me. I find that the tightness across my chest, while not painful, is uncomfortable, so my shoulders droop to relieve the pressure and I slouch. Although I’m more comfortable that way, it makes my whole body ache at the end of the day. It’s just awkward. I must admit that I was getting kind of bored at home, though, so the return to work was good for me. I missed the face-to-face interaction with my friends and co-workers.
I have a desk job, so it isn’t very physically demanding, but I did feel completely pooped after my second day back. Sitting in one spot for most of eight hours is much different than lounging on the couch and it caught up with me. I find that the tightness across my chest, while not painful, is uncomfortable, so my shoulders droop to relieve the pressure and I slouch. Although I’m more comfortable that way, it makes my whole body ache at the end of the day. It’s just awkward. I must admit that I was getting kind of bored at home, though, so the return to work was good for me. I missed the face-to-face interaction with my friends and co-workers. I am now driving and no longer need a chauffeur.
I am now driving and no longer need a chauffeur.
 Hyperbaric oxygen therapy (HBOT) involves the breathing of pure oxygen while in a sealed chamber that has been pressurized at 1-1/2 to 3 times normal atmospheric pressure. –
Hyperbaric oxygen therapy (HBOT) involves the breathing of pure oxygen while in a sealed chamber that has been pressurized at 1-1/2 to 3 times normal atmospheric pressure. – 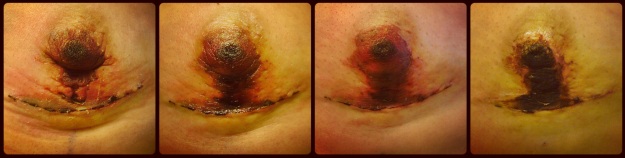
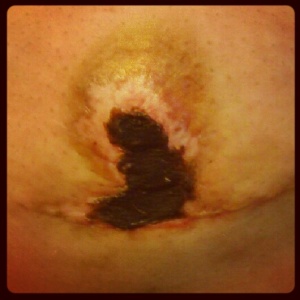

 A couple of days before my prophylactic nipple-sparing bilateral
A couple of days before my prophylactic nipple-sparing bilateral  Breast skin is fragile after mastectomy. If it’s exceptionally thin after the breast tissue is cut away or is handled too roughly, it may die. The same result may occur if the breast surgeon severs too many blood vessels that feed the skin or uses eletrocautery too aggressively and burns the inside of the skin, which may then blister and die.
Breast skin is fragile after mastectomy. If it’s exceptionally thin after the breast tissue is cut away or is handled too roughly, it may die. The same result may occur if the breast surgeon severs too many blood vessels that feed the skin or uses eletrocautery too aggressively and burns the inside of the skin, which may then blister and die.

 Water, water, water. I drink plenty of water. Guava juice is also good and tasty! Bolthouse Farms Passion Orange Guava juice is my drink of choice.
Water, water, water. I drink plenty of water. Guava juice is also good and tasty! Bolthouse Farms Passion Orange Guava juice is my drink of choice.
 Post-op workouts are one thing. Preparing your body before the procedure is another, and just as important. It is the #1 item on my
Post-op workouts are one thing. Preparing your body before the procedure is another, and just as important. It is the #1 item on my