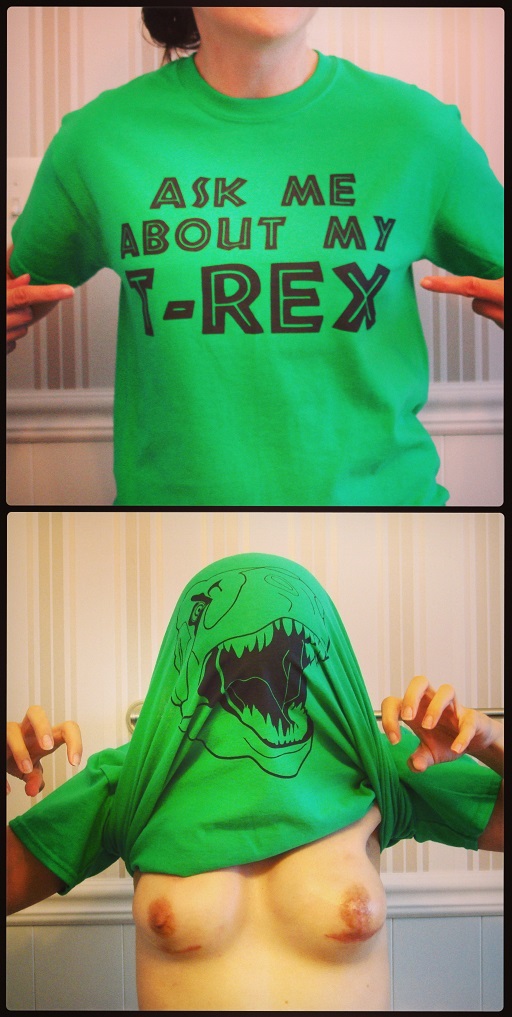
WARNING: NSFW / graphic content below.
Final preparations
 During the last few days before surgery, I made final preparations for the big day. One of them being picking up my dad from the airport. He surprised me the Thursday before surgery by telling me he purchased his ticket to fly in from Europe to spend a month out here and help my husband take care of me. A great relief to have an extra set of hands. It’s nice to have dad here, but I plan on making a quick recovery, so I hope he doesn’t get bored!
During the last few days before surgery, I made final preparations for the big day. One of them being picking up my dad from the airport. He surprised me the Thursday before surgery by telling me he purchased his ticket to fly in from Europe to spend a month out here and help my husband take care of me. A great relief to have an extra set of hands. It’s nice to have dad here, but I plan on making a quick recovery, so I hope he doesn’t get bored!
I received two separate calls from the hospital the day before the procedure confirming we were still a “go.” I got a lot of detailed information about the timeline and what the day would look like. I confirmed that 1. I would be in a private room (space for hubby AND dad to spend the night) and 2. the hospital has wi-fi.
The night before surgery, I made sure the recliner and area around it were ready for my return home. I gathered all of the things mentioned on my checklist, without exception. I packed my hospital bag with all of the necessities and hit the sack early. I was expecting to have a bit of anxiety in the last few days leading up to the surgery, so I had my doctor write me a prescription for Ativan. The bottle is still full. I was a bit nervous, but not as much as I thought I would be.
The morning of my prophylactic bilateral mastectomy

ID and FALL RISK wrist bands
I was told to be at the hospital by 5:30am, with surgery scheduled to start at 7:30am. We arrived a bit early and waited to get checked in. The receptionist confirmed my name and date of birth and tagged me with my wrist band and the handy-dandy “FALL RISK” warning bracelet.
About 30 minutes later, I was called back by the pre-op nurse. She took my vitals, had me change into a Bair Paws gown (nothing underneath), and asked for a urine sample. We went over all of the paperwork, including consent forms I already signed. I was sure to point out that I didn’t consent to residents or fellows performing any part of the procedure, which was noted. She got my compression socks and booties on and hooked up, another nurse came in and got my IV line in, and then hubby and dad were called in to see me.

Compression socks and booties

Incision markings
A few different nurses, the anesthesiologist, and both surgeons stopped by. I mentioned that I would love to not have any nausea once I woke up and they gave me something. The plastic surgeon marked up my chest wall for the smiley face incisions (with his high-tech Sharpie). BTW, I am 5’4″, 125lbs, and 34A.
I spent a few more minutes with the family and then it was time to roll out. I was wheeled to the operating room where I got to meet a few more of the surgical staff. I scooted over to the operating table, got my arms strapped in and that is all I remember.
The surgery took over five hours: three hours for the mastectomy, two and a half for the expander placement. The fam got regular updates from the operating room (five total) via telephone call into the waiting room. Each surgeon came out to speak with them when their piece was over.
Recovery room
I woke up in the recovery room with a nurse watching my vitals. She made sure I was comfortable and wasn’t feeling nauseous. After an hour another nurse came over to wheel me to my room. While he was there prepping, I had a very sudden wave of nausea wash over me. Got an injection of something and an alcohol swab to sniff (this actually helped) . Once I was OK, we made the trip to my room.
I had a bit of a hard time moving to the bed once in the room. The nurse offered his arm and started pulling me over, but that was painful. We decided to just have his arm available and I would pull instead. I think he got impatient and gave me a little yank at the end. I finally settled in and after about 20 minutes my husband and dad came to my room.
I was hooked up to a morphine drip, which delivered a steady flow of the golden juice. I also had a button I could push for an extra kick that could be added (only every 10 mins). The machine kept track of how often extra meds were requested and how many times it actually delivered. That day I had over 20 requests, but only 12 deliveries, if I remember correctly.
I ate crackers and drank a lot of water. I made my first trip to the bathroom around 7pm. Getting out of bed was rough – needed two people to help to and in the bathroom: one to manage the drains and the other to help on the toilet. Although I felt the need to go, I had a rough time making my body obey. I peed in a “hat” that measured the output which was recorded by the nurse. I made a total of four trips to pee the first night, with each one easier than the last.
It only gets better from here! On to Day 1 of recovery.


 For a recap of why/how the expansion process works, see
For a recap of why/how the expansion process works, see 
 What are
What are 
 A couple of days before my prophylactic nipple-sparing bilateral
A couple of days before my prophylactic nipple-sparing bilateral 

 How and when do I empty the drains? A nurse demonstrated how to do this properly. The drains need to be emptied at least twice per day.
How and when do I empty the drains? A nurse demonstrated how to do this properly. The drains need to be emptied at least twice per day.




 On the day of surgery I was on a liquid diet, but it wasn’t even relevant as I was not hungry at all. I downed crackers and a lot of water. Hall’s Vitamin C cough drops helped with the dry mouth and throat. There was a menu in my room and food service staff came around collecting orders. I was worried about constipation, so I focused on high-fiber snacks and meals. Breakfast of choice was plain, bland, tasteless oatmeal. Lunch: dressing-less garden salad. Dinner: mushroom soup.
On the day of surgery I was on a liquid diet, but it wasn’t even relevant as I was not hungry at all. I downed crackers and a lot of water. Hall’s Vitamin C cough drops helped with the dry mouth and throat. There was a menu in my room and food service staff came around collecting orders. I was worried about constipation, so I focused on high-fiber snacks and meals. Breakfast of choice was plain, bland, tasteless oatmeal. Lunch: dressing-less garden salad. Dinner: mushroom soup.
 During the last few days before surgery, I made final preparations for the big day. One of them being picking up my dad from the airport. He surprised me the Thursday before surgery by telling me he purchased his ticket to fly in from Europe to spend a month out here and help my husband take care of me. A great relief to have an extra set of hands. It’s nice to have dad here, but I plan on making a quick recovery, so I hope he doesn’t get bored!
During the last few days before surgery, I made final preparations for the big day. One of them being picking up my dad from the airport. He surprised me the Thursday before surgery by telling me he purchased his ticket to fly in from Europe to spend a month out here and help my husband take care of me. A great relief to have an extra set of hands. It’s nice to have dad here, but I plan on making a quick recovery, so I hope he doesn’t get bored!


 DON’Ts
DON’Ts