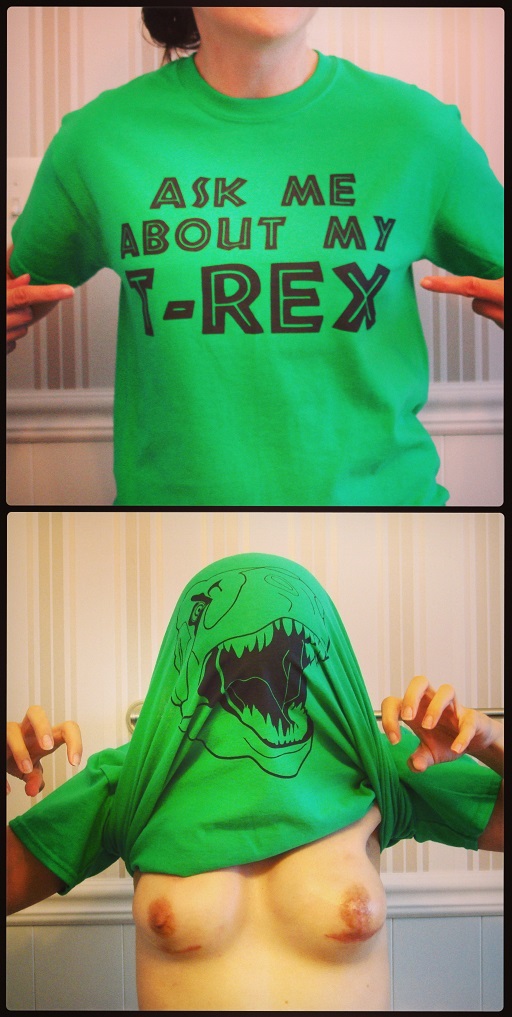
![]() I’d like to take a minute to say welcome to new visitors and subscribers! Thanks for stopping by and checking out my blog. (I know you’re really here for the topless pics 😀 – see: My Photos)
I’d like to take a minute to say welcome to new visitors and subscribers! Thanks for stopping by and checking out my blog. (I know you’re really here for the topless pics 😀 – see: My Photos)
I was recently contacted by a reporter who is writing a story about BRCA and hereditary breast and ovarian cancer (HBOC). I was more than happy to share my story, feedback, and reaction to Angelina Jolie’s New York Times op-ed. I thought adding that here is a great way to give the new readers a summary of my story, so here goes …
Recap
I’m 32, married, no kids (more: About Me). Neither I nor any of my family members carry any of the known BRCA mutations; however breast and ovarian cancer are prevalent in our family. My sister was 28 when she was diagnosed with breast cancer and died a year later. My other sister has a breast biopsy scheduled for next week. My mother is currently undergoing treatment for ovarian cancer.
 Even though I am BRCA mutation negative, I have an increased risk of developing both cancers based on my family history and was faced with the same decision regarding my breast health: choose surveillance, chemoprevention, or surgery. For the past 10 years I chose bi-annual screenings via mammograms, ultrasounds, and a few MRIs. I made a different decision and started planning for a prophylactic bilateral mastectomy when screenings discovered some issues (see: But why?) in March and then June of last year. I underwent the mastectomy in January 2013 and am currently going through the breast reconstruction process, which will end with the second surgery (see: We’re getting there) in September. I have consulted with my doctors about having my ovaries removed and will most likely be seriously considering an oophorectomy in about five years.
Even though I am BRCA mutation negative, I have an increased risk of developing both cancers based on my family history and was faced with the same decision regarding my breast health: choose surveillance, chemoprevention, or surgery. For the past 10 years I chose bi-annual screenings via mammograms, ultrasounds, and a few MRIs. I made a different decision and started planning for a prophylactic bilateral mastectomy when screenings discovered some issues (see: But why?) in March and then June of last year. I underwent the mastectomy in January 2013 and am currently going through the breast reconstruction process, which will end with the second surgery (see: We’re getting there) in September. I have consulted with my doctors about having my ovaries removed and will most likely be seriously considering an oophorectomy in about five years.
When I was preparing for my mastectomy, I spent many hours online looking for first-person accounts of the process and following recovery. I wanted to know every little detail related to the options and decisions I had to make: from which doctors to choose, to what type of reconstruction is available, to how to handle insurance coverage complications. I didn’t find many back then, so I started my blog, sharing my story and photos. I write my blog to give women facing HBOC insight into the experience of a prophylactic mastectomy if they choose to undergo one.
The “Jolie mastectomy”
I was immediately very excited when I read Angelina Jolie’s New York Times op-ed. I could relate to her story, as I had undergone my mastectomy just weeks before she had hers. More importantly, her name is known by millions of people around the world and now her story is too. She accomplished with one op-ed what many organizations have been striving to do for years – bring global awareness to BRCA and HBOC.
The essay described her very personal journey and reasons for making the decision she did. I echo her feeling that choosing to have a mastectomy was not easy, but I have no regrets. Although the decision to have surgery was right for me, Jolie, and countless other women, it is not the right decision for every woman and one that shouldn’t be taken lightly or made without research, consulting with experts/doctors, considering alternative options (screening, chemoprevention, holistic approaches, lifestyle changes), and understanding the consequences. I think it’s important to note that Jolie’s experience is unique. She was fortunate enough to have a relatively complication-free recovery, but there are many women who experience severe complications following their mastectomy.
After her op-ed came the multitude of reactions, commentary, articles, blog posts. Many expressed their support of her decision, but others condemned her. Having made the same decision, it was difficult to not take it all personally. What they were saying about her and the choice she made, they were essentially saying about any woman that made the same decision. I have (thankfully) had support and encouragement from those around me.
Then came the pieces referring to BRCA as the “Angie gene” or the procedure as the “Jolie mastectomy.” I do agree with the post I recently reblogged (see: Semantics) – in a way yes, this trivializes other women, their experiences, their struggles. Women (and men) all over the world deal with the realities of carrying a BRCA mutation every day. The decisions, uncertainty, major life changes, and disruption are a huge part of their lives. For some, not a day goes by that BRCA and cancer aren’t on their mind. Most have watched a loved one deal with cancer and worse. Majority don’t have a famous name or a famous face. Some publicly share their stories via articles, blogs, support groups, and other venues. Jolie hasn’t done anything extraordinary. The “Angie gene?” She’s no pioneer. I have nothing against her and reiterate that I’m ecstatic that she decided to share her story, but she made the same decision thousands of women have made before her and will make after her. Hearing someone say “oh, you had the Jolie mastectomy” makes me cringe and smile at the same time. While I’m peeved by the categorization and potential assumption that I chose this option because she did, I understand that this is the only point of reference some people have and welcome the opportunity to talk about HBOC and BRCA.
3/7/14 update: A few things have changed since I wrote this post in June 2013: mom’s treatment was not effective (or rather TOO effective) and she died in November, my sister’s biopsy results were clear, but she is now prepping for an oophorectomy, my September surgery was NOT my last one,






 Breast skin is fragile after mastectomy. If it’s exceptionally thin after the breast tissue is cut away or is handled too roughly, it may die. The same result may occur if the breast surgeon severs too many blood vessels that feed the skin or uses eletrocautery too aggressively and burns the inside of the skin, which may then blister and die.
Breast skin is fragile after mastectomy. If it’s exceptionally thin after the breast tissue is cut away or is handled too roughly, it may die. The same result may occur if the breast surgeon severs too many blood vessels that feed the skin or uses eletrocautery too aggressively and burns the inside of the skin, which may then blister and die.






 On the day of surgery I was on a liquid diet, but it wasn’t even relevant as I was not hungry at all. I downed crackers and a lot of water. Hall’s Vitamin C cough drops helped with the dry mouth and throat. There was a menu in my room and food service staff came around collecting orders. I was worried about constipation, so I focused on high-fiber snacks and meals. Breakfast of choice was plain, bland, tasteless oatmeal. Lunch: dressing-less garden salad. Dinner: mushroom soup.
On the day of surgery I was on a liquid diet, but it wasn’t even relevant as I was not hungry at all. I downed crackers and a lot of water. Hall’s Vitamin C cough drops helped with the dry mouth and throat. There was a menu in my room and food service staff came around collecting orders. I was worried about constipation, so I focused on high-fiber snacks and meals. Breakfast of choice was plain, bland, tasteless oatmeal. Lunch: dressing-less garden salad. Dinner: mushroom soup.